GLP-1s Walkie Talkie 3/6/24
This is a deep dive into our body’s blood sugar management system. How GLP-1 agonists improve cellular function to reduce body fat and prevent diabetes.
About 38 million Americans have diabetes…that means 10% of the US population has type 2 diabetes.
Type 2 diabetes mostly develops in people over 45 years old. However, the rate of children and teens developing type 2 diabetes is surging at an alarming rate.
WHAT IS DIABETES?
Diabetes is a chronic condition that affects how your body turns food into energy. Basically, diabetes is an endocrine disease that presents when the body cannot regulate blood sugar.
The body breaks down most food into sugar (glucose), releasing it into your bloodstream.
When blood sugar levels rise, it signals the pancreas to release insulin.
WHAT’S INSULIN?
Insulin is a peptide hormone secreted by Beta cells found in pancreatic islets. It maintains normal blood sugar levels by facilitating cellular glucose (sugar) uptake and by regulating carbohydrate (glycogen), lipid, and protein metabolism.
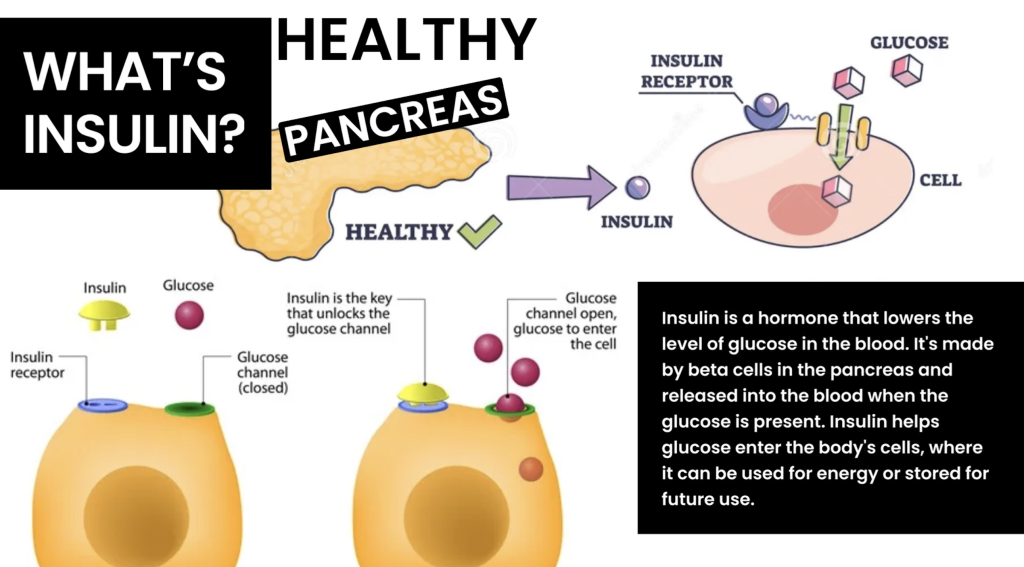
Insulin acts like a key, letting blood sugar into your body’s cells for use as energy.
Insulin binds to sugar in our blood and, through an insulin receptor in our cell membrane, can move sugar from the blood into the cell for energy.
SUGARS TO BALANCE
Glucose is a monosaccharide (one), meaning it’s a single structural carbohydrate unit. Our cells use glucose to make ATP. And the desire of insulin is to move glucose into the cell for energy.
Glucose is a large molecule and can’t pass the cellular membrane without insulin unlocking the glucose channel.
Glycogen is a polysaccharide (many). Meaning it’s a chain of glucose and is considered a starch. Glycogen is stored in our liver.
HOW INSULIN WORKS?
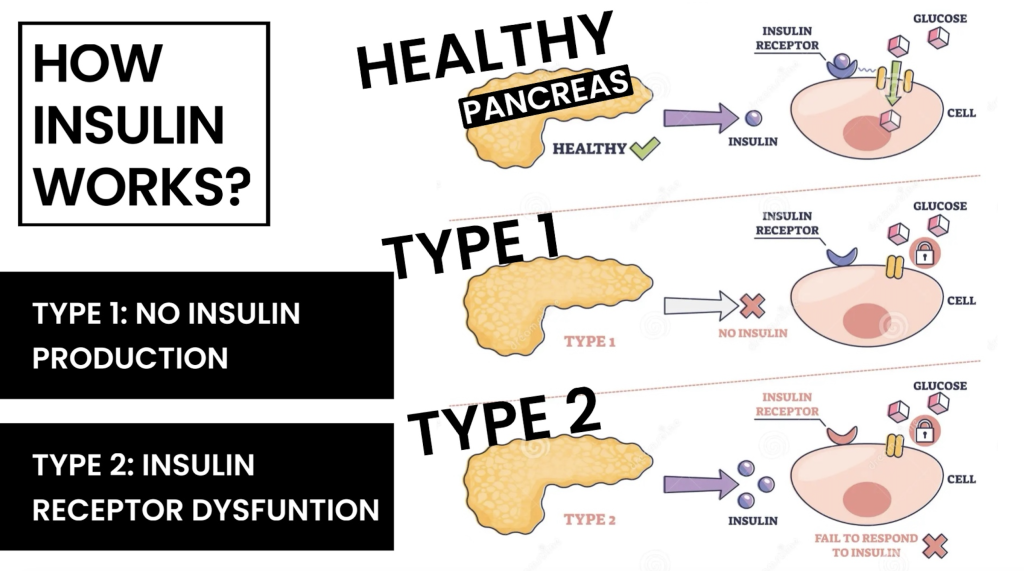
TYPE 1 Diabetes presents when the pancreas doesn’t make insulin. This is why most type 1 diabetics are children. To compensate for this lack of insulin, they inject insulin. The insulin receptor still functions in type 1 diabetes, and Insulin can remove sugar from the blood.
TYPE 2 Diabetes presents when cellular function declines. Your pancreas makes insulin, but the insulin receptor cannot use it. This causes the pancreas to make more insulin until the pancreas burns out and can no longer make insulin.
With diabetes, your body doesn’t make enough insulin or can’t use it as well as it should. When there isn’t enough insulin or cells stop responding to insulin, too much blood sugar stays in your bloodstream. Over time, that can cause serious health problems, such as heart disease, vision loss, and kidney disease.
DIABETES IS AN EPIDEMIC!!!
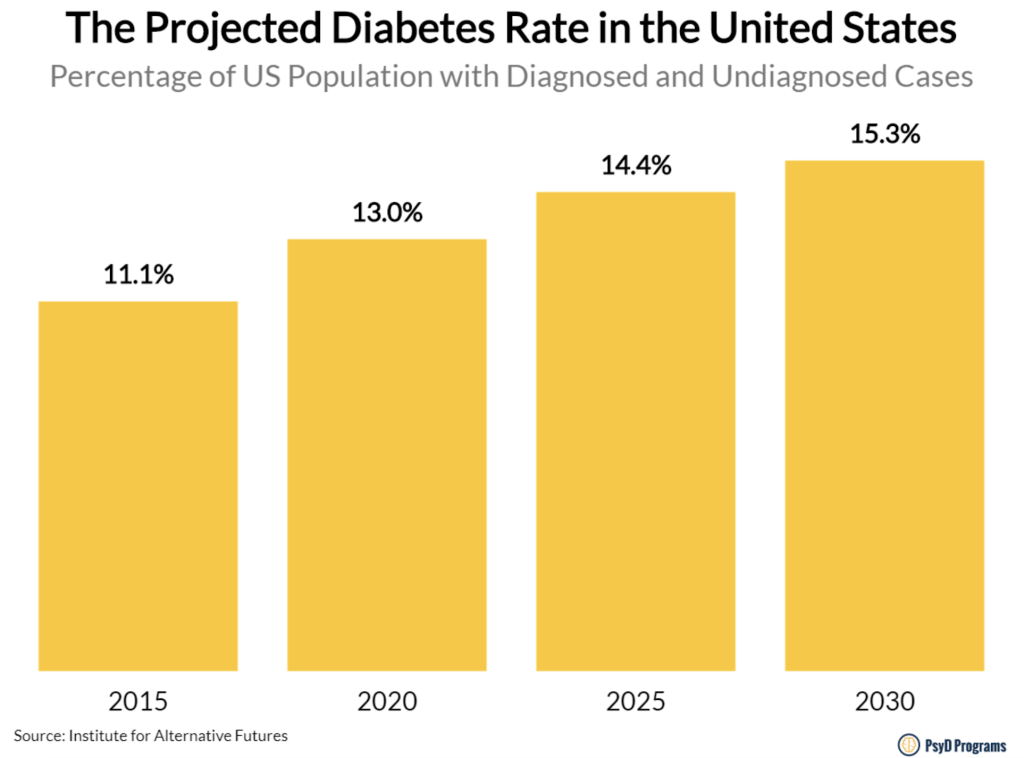
Pre-diabetes means you have a higher-than-normal blood sugar level. It’s not high enough to be considered type 2 diabetes. However, without lifestyle changes, adults and children with pre-diabetes are at high risk for developing type 2 diabetes.
Currently, there are over 100 Million in the US considered pre-diabetic, and by 2030, over 15% of the US will have Type 2 Diabetes.
INSULIN V. GLUCAGON
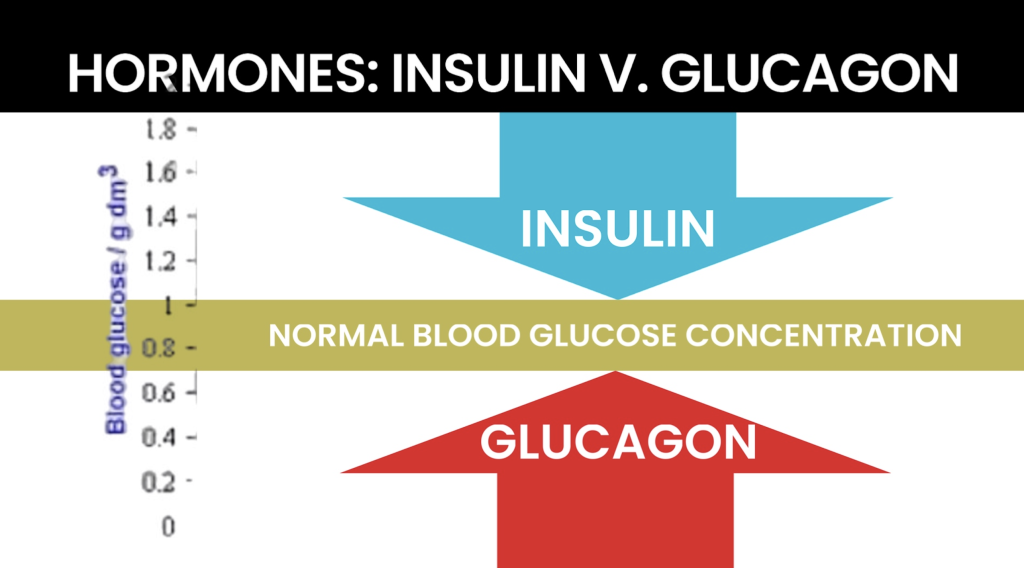
Monitoring blood sugar is a balancing act between Insulin, which wants to remove sugar from the blood, and its counterpart, Glucagon, which wants to release sugar into the blood. We need both hormones working efficiently to maintain balanced blood sugar.
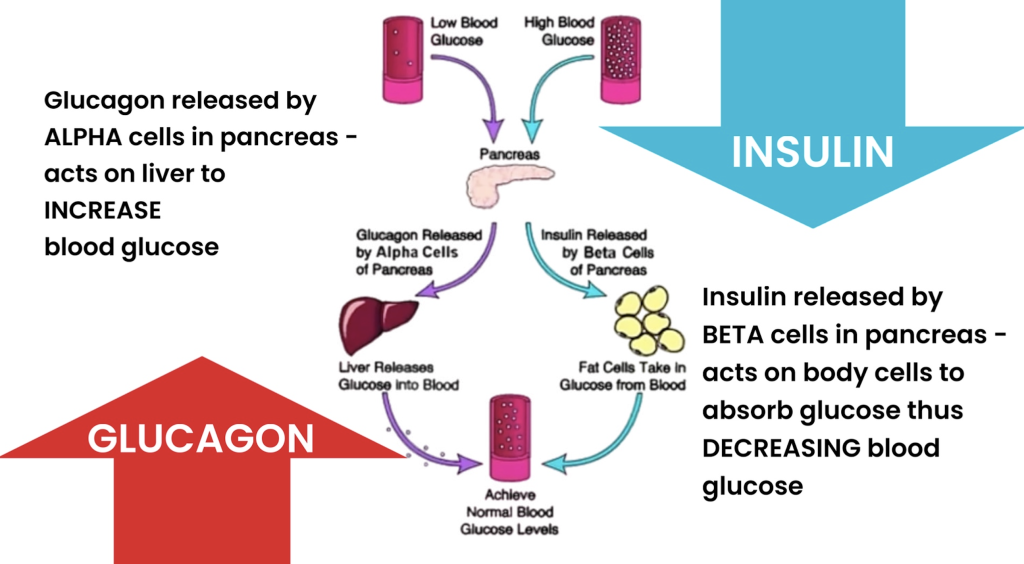
Insulin and Glucagon are created in the pancreas and begin when Beta or Alpha cells are triggered in pancreatic islets.
When our blood sugar is low, alpha cells release glucagon in the pancreas. The pancreas has stores of glycogen (polysaccharide starch). Glucagon breaks the glycogen chain down into single molecules of glucose and releases them into the blood to increase blood sugar.
When glucagon is high, it signals constantly to the liver to release its stored glucose into the blood.
⬆️ Glucagon wants to increase blood sugar.
⬇️ Insulin wants to decrease blood sugar.
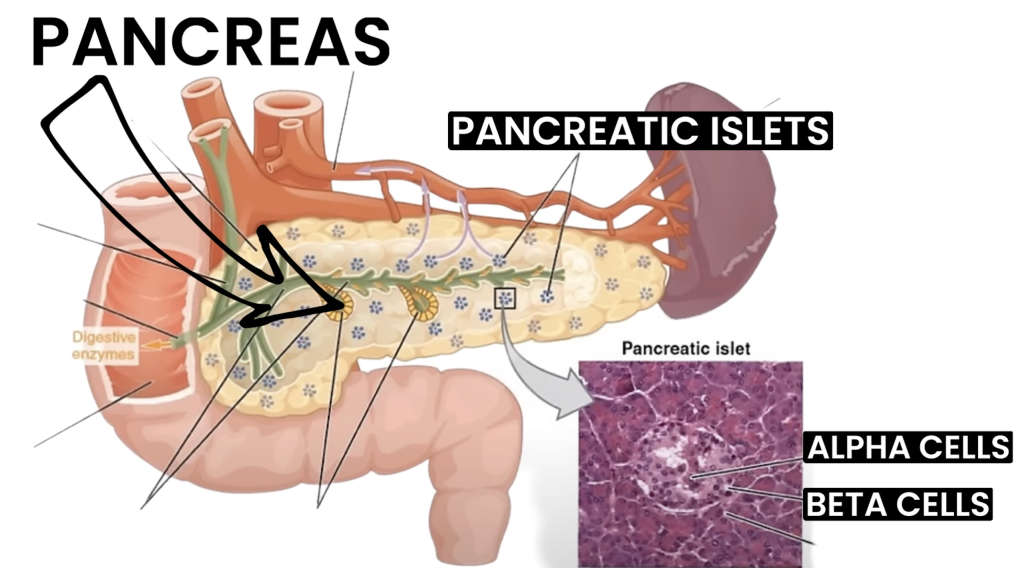
These hormones are triggered by Alpha and Beta cells originating from pancreatic islets inside the pancreas. The Alpha and Beta cells then trigger Insulin or Glucagon hormones to balance blood sugar.
INSULIN IS A PEPTIDE
As explained in the previous peptide, “Walkie-Talkies,” peptides are short-chain amino acids that aid in cellular communication and function. Peptides are used to optimize cellular communication. Insulin is the most widely used peptide for this purpose since 1922.
It’s unclear why some develop Type 2 diabetes while others don’t. However, the issue is that the insulin receptor on the cellular membrane becomes dysfunctional. There is a communication breakdown, and Insulin addresses this dysfunction.
However, the issue with Insulin treating diabetes is that it simply band-aids the issue rather than aiding in the solution. People with dysfunctional insulin receptors, whether they are pre-diabetic or diabetic, want to solve the receptor’s dysfunction so they can solve this endocrine disease.
This is what makes the weight loss peptides, known as GLP-1 Agonists, very exciting; instead of being a band-aid, these popular peptides can restore cellular communication, reversing diabetes.
What are GLP-1 Agonists?
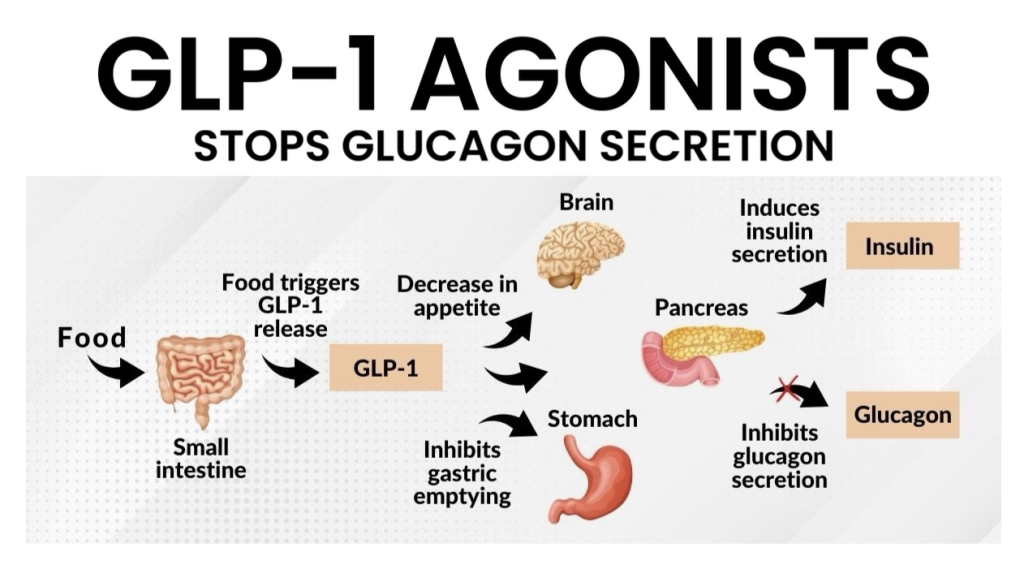
GLP-1 stands for: “Glucagon-Like Peptide 1 agonist”.
GLP-1 is a peptide hormone that exhibits a glucose-lowering effect by stimulating insulin secretion while inhibiting glucagon secretion at the same time.
Patients with diabetes frequently have a deficient glucagon response to hypoglycemia and exhibit an inappropriately high glucagon response to a meal. This dysregulation has been attributed in part to a lack of intraislet insulin, but the exact pathophysiologic mechanisms remain controversial.
From the above excerpt, you can imagine there is a cellular dysfunction for those who gain abnormal weight. Not only can their diet be high in sugar, but their glucagon levels are high, releasing additional sugar and overlading the removal system, insulin.
Besides stabilizing blood sugar, which is helpful for diabetics, the biggest effect is stopping glucagon release. This means you have less blood sugar to clear.
While preventing your liver from releasing more sugar into your blood, it decreases appetite with its ability to work on gut-brain access, which I explained last week when I focused on BCP157.
GLP-1 agonists are used primarily to reduce blood sugar in diabetic patients. However, people who are not yet diabetic but have become insulin-sensitive benefit greatly, too.
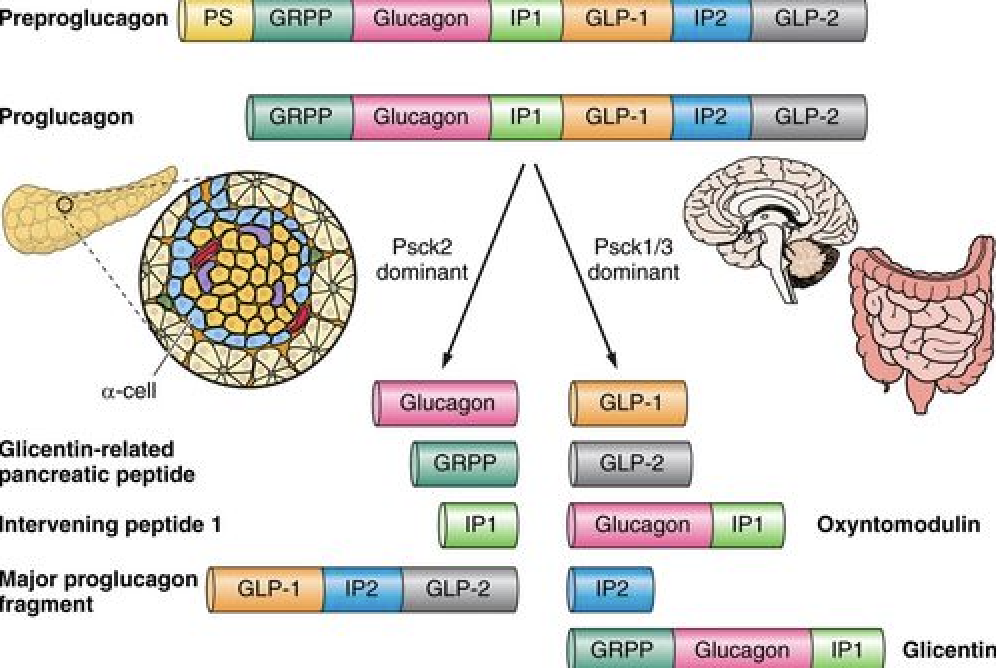
What is the GLP-1 signal peptide?
The GLP-1 hormone is created in the small intestine. It is a 30-amino acid peptide hormone produced in the intestinal epithelial endocrine L-cells by differential processing of proglucagon, the gene that is expressed in these cells.
GLP-1 prevents more glucose from going into your bloodstream.
Which GLP-1 agonists have I tried?
The two GLP-1 agonists I’ve personally used are:
-Liraglutide (brand name Saxenda)
-Semaglutide (brand name Ozempic)
There’s also a similar class of medications called dual GLP-1/GIP receptor agonists. There’s currently one of these medications on the market. It’s called tirzepatide (Mounjaro®). I’ve not tried this weight management peptide, but many who try semaglutide and don’t find sufficient success switch to Tirzepatide and find it to be more powerful.
How do GLP-1s work in the body?
- Triggering insulin release from your pancreas.
- Blocking glucagon secretion
- Slowing stomach emptying: Slower digestion means that your body releases less glucose (sugar) from the food you eat into your bloodstream.
- Increasing how full you feel after eating (satiety): GLP-1 affects areas of your brain that process hunger and satiety.
GLP-1 agonist medications work by mimicking this hormone. In medication terms, an agonist is a manufactured substance that attaches to a cell receptor and causes the same action as the naturally occurring substance. In other words, GLP-1 medications bind to GLP receptors to trigger the effects (or roles) of the GLP-1 hormone. The higher the dose of the GLP-1 agonist, the more extreme the effects.
If you have Type 2 diabetes, the medications help manage your blood sugar by triggering your pancreas to release more insulin. The slowed digestion also helps decrease blood sugar spikes.
The satiety effect of GLP1-agonists reduces your food intake, appetite, and hunger. These combined effects often result in weight loss.
Our bodies make GLP-1, but it is rapidly degraded and has a half-life of only 2 minutes, meaning that only 10-15% of our own GLP-1 reaches circulation intake. In order to increase GLP-1 life span, GLP-1 receptor agonists were developed to survive longer, leading to a stronger effect.
LIRAGLUTIDE v. SEMAGLUTIDE?
Head-to-head randomized controlled trials have shown that semaglutide supports weight loss of around 15%, compared to 5-6% with liraglutide. These studies have also shown that semaglutide reduces blood sugar levels (measured by HbA1c) more effectively than liraglutide by around 0.5%.
TIRZEPATIDE
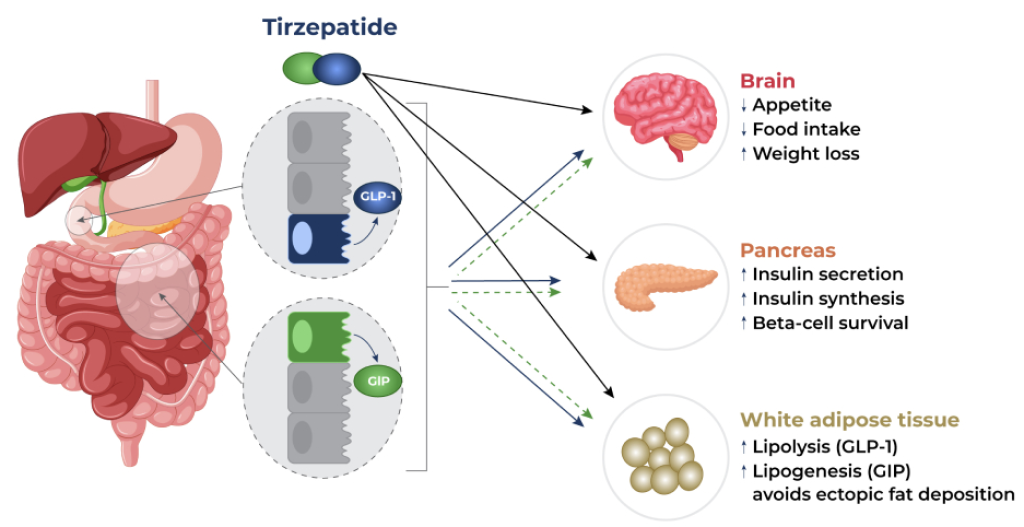
Tirzepatide is a dual agonist that targets both the GLP-1 and glucagon receptors, while Semaglutide is a single GLP-1 receptor agonist.
Tirzepatide differs from semaglutide because it also mimics the GIP hormone, which affects stomach emptying, appetite, and how fat is deposited.
Using tirzepatide resulted in a weight loss of 17.8% (95% CI: 16.3%-19.3%) compared with 12.4% (95% CI: 11.5%-13.4%) for semaglutide.
Despite the similarities between the two incretins, it should be pinpointed that while GIP activity is mainly pancreatic, GLP-1 activity is systemic.
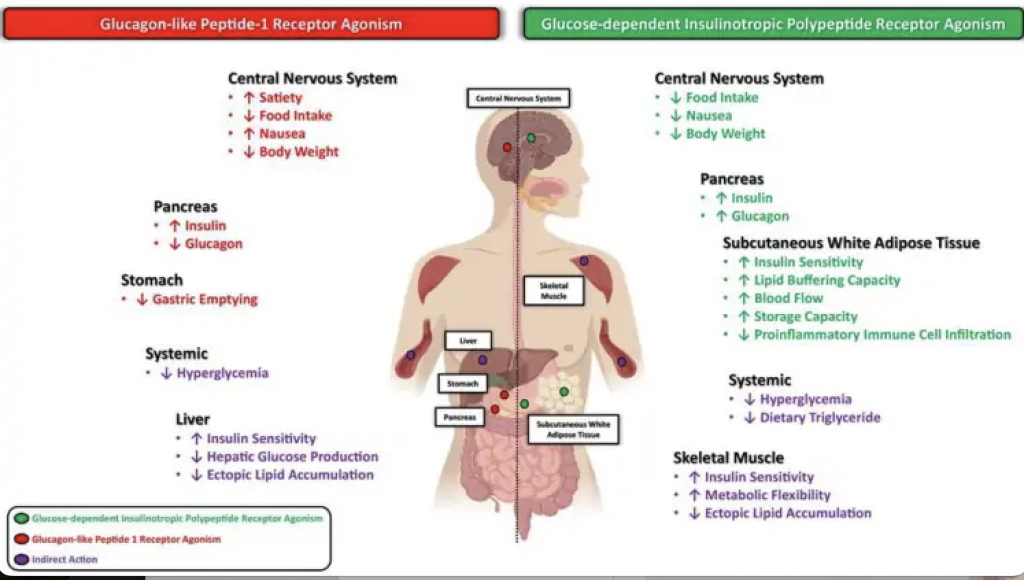
GLP-1 elicits a range of GI, metabolic, and neurological effects, which can be regarded as facilitating nutrient digestion, absorption, and processing. The best-studied function of GLP-1 is as an incretin hormone, acting to potentiate glucose-dependent insulin secretion from pancreatic beta cells.
CONCLUSION
From this deep dive into how our body monitors blood sugar, I’ve learned that first, we become “Insulin Resistant,” meaning that the insulin receptors along our cell membranes do not sense the presence of Insulin, and this causes our pancreas to make more insulin.
By using GLP-1, we can improve insulin resistance and optimize this system. Again, optimizing cell function and communication is the main role all peptides play in our body, and this includes these very popular weight-loss-inducing peptides.
Liraglutide was one of the initial GLP-1, but as medicine has advanced, the GLP-1 offerings have improved. Liraglutide requires a daily injection, posing less compliance, and, based on studies, appears to be less effective at reducing hunger. I used Liraglutide for a period of time; it did cause nausea, so I would dose at night and sleep through that sensation. It helped me maintain, but I wasn’t great and doing my dose daily, so I never saw an effective weight drop.
I tried semaglutide in 2023 and used it for six months to lose 25 lbs. I loved that it was a once-weekly injection. Semaglutide has a half-life of 7 days, whereas liraglutide has only 24 hours.
With the addition of the dual GLP-1/GIP receptor agonists, Tirzepatide appears to be the most effective at reducing weight, fat storage, reduction of glucagon, and building back insulin sensitivity. Tirzepatide, like semaglutide, also has a seven-day half-life, which means a once-weekly injection is easier for most people to find compliance with.
SOURCES:
ARTICLES
VIDEOS
PODCASTS



Is there a way to microdose Mounjaro due to the design of the pen? I have used Ozempic at .25/wk and it’s now soldout on Fillerhouse. I would like to try Mounjaro but at a minimal dose to avoid nausea as I am at a comfortable weight but want to maintain with a low dose. Thanks!
Hello Ava! Members in the Natural Kaos App have shared their experiences. You can find similar posts in the App.